In today’s digital age, it’s easy to see how too much of anything can be detrimental to our health. Too much television can strain the eyes; too many exposures to loud music can damage hearing; too much texting can lead to arthritic thumbs. But who would have guessed that too much medicine could be a bad thing?

What’s hiding in your nose is more important than you thought
(Credit: bienestar.salud180.com)
According to a recent report in USA Today, researchers believe that we are entering a “Post Antibiotic Age,” where commonly prescribed medicines will no longer work to cure harmful bacterial infections. The reason? Overexposure. Doctors have been prescribing too many antibiotics for too long.
“Doctors and patients desperately need new antibiotics to replace the ones that are losing their effectiveness,” claims Lisa Proctor, program director of the Human Microbiome Project at the National Institutes of Health. Not only are antibiotics hard to develop, but they can also cost up to $1 billion per drug. What’s more, unlike drugs that are taken for many years or a lifetime, antibiotics are prescribed for a relatively short period of time. Thus, drug companies have little to no economic incentive to invest in manufacturing them, which has resulted in a steady production decline. (The newest class of antibiotics was released over 30 years ago.) According to the Centers for Disease Control and Prevention, at least 2 million Americans develop antibiotic-resistant infections each year, and 23,000 of them die.
That’s where the nose comes in. While most antibiotics are produced from fungi or soil bacteria, German scientists have recently developed a new antibiotic from a strain of the bacterium “Staphylococcus aureus” found in the human nose. The bacterial strain is present in only about 10 percent of the world’s population, but scientists believe that it may be the key to saving thousands of lives.
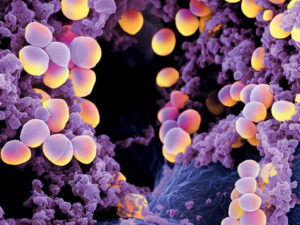
Staphylococcus aureus bacterium
(Credit: biologyuofteeb.blogspot.com)
While the new antibiotic, named lugdunin, has only been tested on rats, researchers have found that it could cure infections caused by methicillin-resistant Staphylococcus aureus, or MRSA. MRSA is resistant to a variety of medications, and often leads to serious, sometimes life-threatening infections in the skin, bloodstream, heart, and lungs.
Although human studies of lugdunin are not yet underway, this profound discovery may pave the way to better antibiotics and more cures. And too much of that is never a bad thing!

 How Your Schnoz may be the Biggest Weapon against the “Post Antibiotic Age”
How Your Schnoz may be the Biggest Weapon against the “Post Antibiotic Age”


 Final Messages of the Dying
Final Messages of the Dying
 Will I Die in Pain?
Will I Die in Pain?















